When chronic sinus issues turn your daily life into a cycle of congestion, pain, and frustration, the idea of surgery often arises as a potential solution. For many, simply hearing "sinus surgery" can trigger anxiety, but Understanding Sinus Surgery & Indications is the first step toward clearer breathing and better health outcomes. This comprehensive guide will demystify the process, from why it might be recommended to what you can expect every step of the way, empowering you to make informed decisions with confidence.
At a Glance: Key Takeaways on Sinus Surgery
- Purpose: To clear obstructions, improve drainage, and correct structural issues in the sinuses, ultimately restoring normal breathing and reducing chronic symptoms.
- Primary Candidates: Individuals with severe chronic sinusitis, recurrent acute infections, nasal polyps, deviated septums, or other structural abnormalities that haven't responded to conservative treatments.
- Most Common Approach: Functional Endoscopic Sinus Surgery (FESS) and related endoscopic techniques, using a small scope through the nostrils.
- Not a First Resort: Surgery is typically considered after other treatments like medication, lifestyle changes, and allergy management have been exhausted.
- Team Effort: Performed by an otolaryngologist (ENT), sometimes with an oral and maxillofacial surgeon.
- Preparation is Key: Pre-operative tests, medication adjustments, and specific instructions are vital for a smooth process and successful outcome.
- Recovery Varies: While initial recovery is 1-2 weeks, full healing can take several months. Adherence to post-operative care is crucial.
- High Success Rate: Most patients (80-90%) experience significant improvement, though recurrence can happen, sometimes requiring revision surgery.
The Sinus Story: Why We Have Them (and Why They Go Wrong)
Imagine your sinuses as an intricate network of air-filled caves behind your cheekbones, forehead, between your eyes, and behind your nose. These four pairs of cavities – maxillary, frontal, ethmoid, and sphenoid – play a vital role beyond just making your head lighter. They warm and humidify the air you breathe, produce mucus that traps pollutants, and even contribute to your voice's resonance.
Ideally, mucus flows freely from these sinuses through small openings (ostia) into your nasal passages, where it's eventually swallowed. But when these drainage pathways become blocked or inflamed, trouble begins. Allergies, infections, structural abnormalities, or growths can cause mucus to back up, creating a breeding ground for bacteria. This leads to the painful pressure, congestion, and difficulty breathing characteristic of sinusitis, a condition that impacts millions annually. For many, lifestyle adjustments, medications, and other non-surgical therapies can bring relief. But when these methods repeatedly fail, and symptoms persist or worsen, it’s time to consider a more direct intervention.
When Conservative Care Isn't Enough: Indications for Sinus Surgery
Sinus surgery is never the first option. It's typically reserved for situations where chronic or severe sinus problems have become refractory to all other medical treatments. If you've tried antibiotics, nasal corticosteroids, saline rinses, allergy management, and decongestants for months or even years with little to no lasting relief, your doctor might suggest that it's time to explore surgical solutions.
Here are the primary indications that suggest you might benefit from sinus surgery:
Chronic Sinusitis (Refractory & Recurrent Acute)
This is the most common reason for sinus surgery. If you've been diagnosed with chronic sinusitis, meaning your symptoms (facial pain/pressure, congestion, discharge, reduced sense of smell) have lasted for 12 weeks or more despite medical management, surgery can be life-changing. Similarly, if you experience recurrent acute sinusitis—multiple severe sinus infections per year that respond poorly to antibiotics—surgery may be indicated to open up the natural drainage pathways, allowing for better ventilation and easier mucus clearance. The goal is to break the cycle of infection and inflammation.
Nasal Polyps
These soft, non-cancerous growths inside the nose and sinuses are a frequent culprit behind chronic congestion, reduced sense of smell, and post-nasal drip. Polyps can grow large enough to completely block sinus openings, leading to chronic infections. While steroid sprays can sometimes shrink them, polyps often recur. Surgery (nasal polypectomy) effectively removes these obstructions, restoring airflow and improving sinus function. For some individuals, this may be an ongoing battle, as polyps can grow back.
Deviated Septum
The septum is the wall of cartilage and bone that divides your nose into two nostrils. A deviated septum means this wall is off-center, making one nasal passage significantly smaller than the other. This structural issue can impair breathing, contribute to chronic sinus infections by blocking drainage, and cause nosebleeds. A septoplasty, a common surgical procedure, corrects this deviation, straightening the septum to improve airflow and facilitate proper sinus drainage. This is often performed in conjunction with other sinus procedures.
Sinus Mucoceles, Pyoceles, and Other Structural Abnormalities
Sometimes, the issue isn't just inflammation but a physical blockage.
- Mucoceles are cysts filled with mucus that can slowly expand, eroding bone and causing pressure on surrounding structures like the eye socket.
- Pyoceles are mucoceles that have become infected, filled with pus.
- Structural abnormalities of the ostiomeatal complex refer to deformities in the narrow drainage pathways where several sinuses connect. These can be congenital or develop over time, creating bottlenecks that prevent proper ventilation and drainage, setting the stage for recurrent infections. Surgery aims to remove these blockages and widen the natural openings.
Sinus Tumors, Biopsies, and Specialized Procedures
While less common, sinus surgery can also be indicated for:
- Removal of benign or malignant tumors found within the sinus cavities.
- Biopsies to diagnose suspicious growths.
- Procedures involving the eye socket, such as optic nerve decompression (to relieve pressure on the optic nerve) or orbital decompression (to treat bulging eyes, often due to thyroid eye disease).
- Dacryocystorhinostomy (DCR), a procedure to open a blocked tear duct, often performed endoscopically through the nose.
In essence, if your sinuses are consistently inflamed, blocked, or structurally compromised, and conservative treatments aren't working, sinus surgery offers a path to alleviate suffering and restore respiratory health. Understanding these indications is the first step in weighing sinus surgery pros and cons and deciding if it’s the right option for you.
Navigating the Options: Types of Sinus Surgery
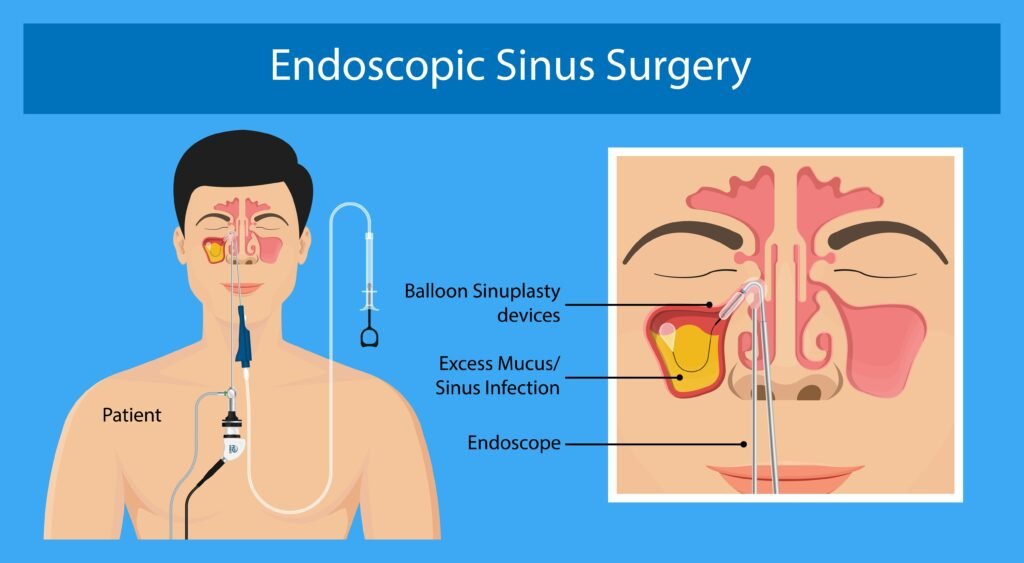
Sinus surgery isn't a single procedure; it's an umbrella term for a variety of techniques tailored to address specific problems. The vast majority of these are performed using an endoscope—a thin, lighted tube with a camera—inserted through your nostrils. This minimally invasive approach means no external incisions, less pain, and quicker recovery. Open surgery is rare and typically reserved for complex cases where infections have spread or for specific structural repairs.
Let's explore the common types:
Endoscopic Sinus Procedures: The Modern Standard
These procedures are usually performed by an otolaryngologist (ENT) and utilize a high-definition endoscope to visualize and operate within the intricate sinus anatomy.
- Functional Endoscopic Sinus Surgery (FESS): This is the most common and versatile approach, often used as a general term. FESS isn't a single procedure but a combination of techniques performed endoscopically to open and enlarge the natural drainage pathways of the sinuses. The surgeon removes inflamed or diseased tissue, bone, or polyps that are blocking the sinus openings. It's often personalized to your specific anatomy and issues.
- Balloon Sinuplasty: A newer, less invasive endoscopic technique. Instead of removing tissue or bone, a tiny balloon catheter is inserted into the blocked sinus opening and inflated. This gently remodels and widens the passage, improving drainage without cutting or removing tissue. It's often used for less severe blockages or in combination with FESS.
- Ethmoidectomy: This procedure targets the ethmoid sinuses, located between your eyes. The surgeon removes the thin bony partitions between these small, air-filled cells to create a larger, unified cavity, allowing for better drainage and ventilation.
- Maxillary Antrostomy: This involves widening the natural opening of the maxillary sinuses (located behind your cheekbones) to improve drainage. Sometimes, an additional opening called a "middle meatal antrostomy" is created if the natural opening is too small or blocked.
- Nasal Polypectomy: Specifically focuses on the endoscopic removal of nasal polyps that obstruct nasal breathing and sinus drainage.
- Septoplasty: Addresses a deviated septum. During this procedure, the surgeon straightens the cartilage and bone of the septum, often by removing small pieces, to improve airflow through both nostrils. This is frequently combined with FESS if sinus issues are also present.
- Sphenoidectomy: This opens the sphenoid sinuses, located deep within the skull behind the eyes, to drain mucus or remove growths. Due to their proximity to vital structures like the optic nerve and carotid arteries, this procedure requires extreme precision.
- Turbinectomy (or Submucous Resection of Turbinates): The turbinates are structures along the side walls of your nose that warm and humidify air. If they become enlarged (hypertrophied), they can block airflow. A turbinectomy involves removing part or all of the turbinate bone or shrinking the soft tissue surrounding it to improve breathing.
- Sinusotomy: A general term meaning "making an incision into a sinus." It's often used in endoscopic contexts to refer to creating a new opening or enlarging an existing one to allow for drainage and reduce inflammation.
- Endoscopic Skull Base Surgery: A highly specialized endoscopic procedure used to remove abnormal growths on the underside of the brain or at the skull base, often in collaboration with neurosurgeons. This highlights the advanced capabilities of modern endoscopic techniques.
Open Surgical Approaches: For Specific, Complex Needs
While endoscopic surgery is the norm, open surgery is occasionally necessary, particularly for very severe infections, large tumors, or when endoscopic access is insufficient.
- Caldwell-Luc Surgery: A classic open procedure primarily for the maxillary sinus. The surgeon makes an incision under the upper lip, through the gum, to create an opening in the bone above the teeth. This allows for direct access to remove diseased tissue, cysts, or foreign bodies from the maxillary sinus. It's less common today due to FESS but is still used for specific indications, like widespread fungal infections or certain types of tumors. This procedure is generally avoided in young children due to potential impact on secondary tooth growth.
- Maxillary Sinus Floor Augmentation ("Sinus Lift"): Though not strictly a sinus treatment in the traditional sense, this is an open procedure often performed by oral and maxillofacial surgeons or periodontists. It involves grafting bone material to the floor of the maxillary sinus to create enough bone height for dental implants in the upper jaw. While it involves the sinus, its purpose is dental.
- Maxillotomy: An endoscopic procedure to section the maxillary sinus for repositioning, often used in reconstructive or tumor removal cases where direct access to the sinus is required for more extensive work.
Your surgeon will determine the most appropriate surgical technique—or combination of techniques—based on your specific anatomy, diagnosis, and the extent of your sinus disease, ensuring the best possible outcome for your situation.
The Surgical Journey: What to Expect, Step-by-Step
Embarking on sinus surgery can feel like a significant undertaking, but understanding each phase of the journey can ease anxieties. From the initial evaluation to the moment you wake up, here’s a clear roadmap.
Is It Right for You? The Pre-Surgery Evaluation
Before surgery is even considered, your ENT will conduct a thorough assessment. This isn't just about looking at your nose; it's about understanding the intricate architecture of your sinuses and identifying precise targets for intervention.
- Detailed Medical History and Physical Exam: Your doctor will ask about your symptoms, their duration, previous treatments, allergies, and overall health. A physical exam will include a visual inspection of your nasal passages.
- Nasal Endoscopy: This in-office procedure involves inserting a thin, flexible scope with a light and camera into your nostrils. It allows the surgeon to directly visualize the nasal passages, turbinates, septum, and sinus openings, checking for inflammation, polyps, or anatomical blockages. It’s quick and usually well-tolerated with a topical numbing spray.
- CT Scan (Computed Tomography): This is the gold standard for imaging sinuses. A CT scan provides detailed cross-sectional images of bone and soft tissue, offering a precise 3D map of your sinus anatomy. It helps identify the exact location and extent of blockages, infections, and any structural abnormalities, guiding the surgical plan and preventing damage to nearby nerves and blood vessels.
- MRI Scan (Magnetic Resonance Imaging): Less common for routine sinus surgery but may be used to differentiate between soft tissue growths (like polyps or tumors) and fluid retention, or if there's concern about the spread of infection beyond the sinuses.
- Other Potential Tests: Depending on your symptoms, your doctor might recommend rhinomanometry (measures nasal airflow), nasal cytology (examines cells from the nose), or olfactory testing (e.g., UPSIT - University of Pennsylvania Smell Identification Test) to assess your sense of smell.
These diagnostic tests are crucial for mapping out a personalized surgical plan, ensuring the surgeon has a comprehensive understanding of your unique anatomy.
Gearing Up: Preparing for Your Procedure
Once surgery is scheduled, your surgeon's office will provide detailed pre-operative instructions, typically weeks in advance. Following these diligently is paramount for your safety and the success of the operation.
- Pre-Operative Appointment: You’ll meet with your surgeon to review the surgical plan, discuss potential risks, and ensure all your questions are answered.
- Medication Review:
- Bleeding Risks: Crucially, you’ll need to stop certain medications that thin the blood. This includes oral NSAIDs (aspirin, ibuprofen, naproxen, celecoxib, diclofenac), St. John's wort, and high-dose vitamin E, usually for up to two weeks before surgery. Anticoagulants like warfarin (Coumadin) or clopidogrel (Plavix) typically need to be stopped five days prior, under the guidance of your prescribing doctor. Always inform your surgeon of all medications, supplements, and herbal remedies you are taking.
- Other Medications: Your surgeon will advise which other medications you can continue and which to stop.
- Fasting Instructions: You will be required to fast from midnight the night before surgery. This means no food, and only approved sips of water until four hours pre-op, to prevent complications related to anesthesia.
- Smoking Cessation: If you smoke, you'll be advised to stop at least 48 hours before and after surgery. Smoking significantly impairs healing and increases complication risks.
- Arrange for Transport: You will not be able to drive yourself home after surgery due to the effects of anesthesia. Arrange for a trusted adult to pick you up and stay with you for the first 24 hours.
- Logistics: Plan to wear comfortable, loose-fitting clothing. Leave valuables at home. Remove contacts, hearing aids, dentures, and any nose piercings before arriving at the surgical center. Bring your insurance card and photo ID.
Your Surgery Day: From Arrival to Anesthesia
The day of surgery can feel a bit like a whirlwind, but the medical team will guide you through each step.
- Morning Prep: You may be asked to wash with an antiseptic soap (like Hibiclens) the night before and the morning of surgery. Do not apply makeup, lotion, deodorant, or fragrance. If you have a thick mustache, trimming it might be recommended. If advised by your surgeon, use an over-the-counter decongestant nasal spray (e.g., Afrin) 1-2 hours before arriving at the facility to help reduce swelling.
- Arrival: Arrive at the hospital or surgical center 15-30 minutes before your scheduled time to complete necessary paperwork.
- Pre-Op Area: You'll be escorted to a pre-operative area. Here, you'll change into a hospital gown. Nurses will take your vital signs (blood pressure, heart rate, temperature), attach ECG probes to monitor your heart, clip a pulse oximeter to your finger, and insert an IV line into your arm. This IV will be used for fluids and medications, including anesthesia. You’ll meet with your surgeon and the anesthesiologist to discuss any last-minute questions and confirm your understanding of the procedure and anesthesia plan.
Inside the OR: How Sinus Surgery is Performed
Once in the operating room, you'll be positioned supine (lying on your back). The type of anesthesia will vary based on the procedure and your preferences:
- Local Anesthesia with IV Sedation ("Twilight Sleep"): You'll be relaxed and drowsy but conscious enough to respond to commands. This is common for less complex endoscopic procedures.
- General Anesthesia: You will be completely unconscious and unaware of the procedure. This is typical for more extensive endoscopic surgeries or any open procedures.
For Endoscopic Surgery: - The surgical site (inside your nostrils) will be prepped with a solution containing lidocaine (for numbing) and epinephrine (to constrict blood vessels and minimize bleeding).
- The surgeon inserts the endoscope into your nostrils. The live video feed from the endoscope is displayed on a monitor, allowing the surgeon to navigate the intricate anatomy with precision.
- Specialized micro-surgical instruments are used through the nostrils to remove polyps, inflamed tissue, bone, or to enlarge drainage pathways as pre-planned.
- Once the procedure is complete, your surgeon may insert a dissolvable spacer (like an absorbable gel or sponge) or soft nasal packing/splints to help support the newly opened passages, absorb any residual bleeding, and prevent scar tissue from forming.
For Open Surgery (e.g., Caldwell-Luc): - This approach is less common but involves an external incision. For maxillary sinus access, the surgeon typically lifts your upper lip and makes an incision in your gum line. A small hole is then cut in the bony plate above your teeth to access the sinus cavity directly.
- Diseased tissue, cysts, or foreign bodies are removed.
- The incisions are then closed with dissolvable sutures.
The length of the surgery varies widely depending on the complexity of your condition, from about 30 minutes for a simple balloon sinuplasty to several hours for extensive FESS or open procedures.
Waking Up: Immediate Post-Surgery Recovery
After your surgery, you'll be moved to a post-anesthesia care unit (PACU) where nurses will monitor your vital signs as you gradually wake up.
- Initial Sensations: It's normal to feel some pain, pressure in your mid-face, dizziness, and significant nasal congestion. You might also experience a dull headache.
- Pain Management: You'll receive pain medication to manage discomfort.
- Monitoring: Nurses will closely monitor you for any immediate complications, such as excessive bleeding.
- Discharge: Once you are fully awake, your vital signs are stable, and your pain is controlled, you'll be given discharge instructions and released into the care of your pre-arranged driver. Sinus surgery is typically an outpatient procedure, meaning you go home the same day.
The Road to Healing: Post-Surgery Care & Long-Term Outcomes
The success of your sinus surgery hinges significantly on your commitment to post-operative care. This phase is critical for proper healing, preventing complications, and ensuring long-lasting relief.
The First Few Days: Managing Discomfort and Bleeding
The initial 24-72 hours post-surgery are the most critical for managing symptoms and starting the healing process.
- Pain and Discomfort: Expect a headache, a burning sensation in your nose, and pressure in your mid-face. You might also experience mild nausea from the anesthesia. Pain medications (typically acetaminophen/Tylenol; avoid NSAIDs unless specifically cleared by your surgeon) will help.
- Nasal Bleeding: Some bleeding from the nose is very common. It can range from light spotting to more significant oozing, especially for the first 24-48 hours. You may also notice blood-tinged discharge or dark blood from your mouth (swallowed blood). Less commonly, you might experience a black eye or temporary facial/gum numbness, particularly with open procedures like Caldwell-Luc.
- Congestion: Your nose will feel very congested, similar to a severe cold, due to swelling and any packing/spacers.
- Bad Breath: This can occur due to blood in the back of your throat.
- Rest: Take it easy for the first 1-2 days. Elevate your head with extra pillows while sleeping to help reduce swelling and bleeding.
- Saline Nasal Spray: Use an isotonic saline nasal spray every 3-4 hours (as directed by your surgeon) to keep your nasal passages moist and aid in clearing blood clots and crusts.
- Crucial Don'ts:
- DO NOT blow your nose for at least one week. This can dislodge clots, cause bleeding, and potentially lead to serious complications. If you must sneeze, do so with your mouth open.
- DO NOT clean your nostrils or attempt to remove any nasal packing, splints, or tubes unless explicitly approved by your surgeon. These are vital for healing and support.
- DO NOT engage in strenuous activities, heavy lifting, or bending over for at least 1-2 weeks, as these can increase blood pressure and risk bleeding.
If you had open surgery through the mouth (e.g., Caldwell-Luc), brush and floss your teeth normally but avoid the treated area. Rinse with an oral antiseptic three times daily. Apply a cold compress (10-15 minutes on, 10-15 minutes off) to your cheeks or forehead to help with swelling.
Week by Week: Aiding Your Recovery
While you might feel well enough to return to work or light activities within 1-2 weeks, full recovery for your sinuses can take 3-4 months. Consistent follow-up care and adherence to instructions are vital.
- Saline Irrigation: Once any nasal packing or tubes are removed (usually at your first follow-up), your surgeon will likely recommend irrigating your sinuses twice daily with a saline rinse or neti pot. This helps flush out crusts, mucus, and debris, promoting cleaner, faster healing and preventing scar tissue.
- Managing Nosebleeds: If you experience a nosebleed, sit upright, lean slightly forward, and pinch your nostrils firmly for 10-15 minutes. An over-the-counter decongestant nasal spray like Afrin can sometimes help stop stubborn bleeding, but use sparingly and only if cleared by your surgeon.
- Medication Restrictions: Avoid steroid or antihistamine nasal sprays for at least two weeks post-surgery, as they can impede healing and dry out nasal passages. Discuss with your doctor when it's safe to resume any usual nasal medications.
- CPAP Machines: If you use a CPAP machine for sleep apnea, your surgeon may advise temporarily discontinuing its use, or adjusting its pressure, to avoid disrupting the healing sinuses.
- Monitor for Infection: Normal post-surgical discharge can be thick, white, or pinkish/brownish. However, seek immediate medical attention if you experience:
- Greenish-yellow and/or foul-smelling discharge.
- High fever (over 101.5°F or 38.6°C).
- Chills.
- Significantly increased pain or swelling.
- These are signs of a potential infection.
Potential Bumps in the Road: Understanding Risks and Complications
While sinus surgery is generally safe, especially with modern endoscopic techniques, it's crucial to be aware of potential risks. Major complications with endoscopic surgery are uncommon, affecting only about 1% to 3% of procedures. Open surgery, due to its more invasive nature, has a higher reported complication rate, around 19%.
Specific risks associated with sinus surgery include:
- Temporary Facial or Teeth Numbness/Pain: Especially after maxillary sinus procedures.
- Severe Nasal Bleeding: While some bleeding is normal, excessive bleeding requiring hospitalization or a blood transfusion is a rare but serious complication.
- Anosmia (Loss of Smell): This can be temporary or, in very rare cases, permanent. It can also lead to ageusia (loss of taste), as smell is closely linked to taste perception.
- Septal Perforation: A hole developing in the septum, which can cause whistling, crusting, or nosebleeds.
- Vision Problems: Extremely rare but serious complications can include double vision or, in the most severe cases, permanent vision loss, due to the close proximity of the sinuses to the eyes and optic nerve.
- Cerebrospinal Fluid Rhinorrhea (CSF Leak): A leak of brain fluid from the nose. This is very rare but requires immediate medical attention to prevent meningitis.
- Meningitis: An infection of the membranes surrounding the brain and spinal cord, a serious but extremely rare complication, usually secondary to a CSF leak or uncontrolled infection.
Your surgeon will discuss these risks with you in detail during your pre-operative consultation, ensuring you understand them thoroughly before proceeding.
When Surgery Isn't the Answer: Contraindications
There are specific situations where sinus surgery may be delayed, avoided, or where one type of surgery is preferred over another:
- Active Infection: Surgery is typically postponed if you have an active sinus infection, as it can increase the risk of spreading the infection. Antibiotics will be prescribed first.
- Prior Severe Reaction to General Anesthesia: For patients with a history of severe adverse reactions, alternative anesthesia methods or different treatment approaches may be considered.
- Orbital Abscess or Pott's Puffy Tumor: In these severe cases where infection has spread to the eye socket or facial bones, open surgery is often preferred over endoscopic techniques to ensure complete drainage and removal of infected material.
- Age Considerations for Children:
- Endoscopic surgery is less successful in children under age 3 and is often delayed.
- For severe sinusitis in children under 6, adenoidectomy (removal of adenoids) is often the preferred first surgical option, as enlarged adenoids can contribute significantly to sinus issues in this age group.
- Certain open procedures, like Caldwell-Luc surgery, are avoided in young children due to the potential impact on developing secondary teeth.
Beyond the Operating Room: Life After Sinus Surgery
The goal of sinus surgery is not just to fix a problem, but to significantly improve your quality of life. For most patients, this becomes a reality.
Follow-Up Care: Maintaining Your Progress
Your recovery journey extends beyond the initial healing phase. You'll have several follow-up appointments with your surgeon.
- First Follow-Up: Typically scheduled 1-2 weeks after surgery, this appointment allows your surgeon to check on your healing, remove any remaining packing or splints, and clear any crusts or clots from your nasal passages. This "debridement" is a normal and necessary part of post-op care.
- Subsequent Appointments: You may have multiple appointments and repeat CT or MRI scans over several months to ensure healing is progressing well and that the sinus passages remain open. Olfactory tests may also be repeated to track improvement in your sense of smell.
These appointments are crucial for identifying and addressing any potential issues early, such as scar tissue formation or recurrent polyps, and for guiding your long-term management strategy.
Outcomes: What You Can Expect Long-Term
The vast majority of individuals who undergo sinus surgery experience significant improvement or full resolution of their symptoms. Studies show that 80% to 90% of patients report better breathing, reduced facial pain, fewer infections, and an improved quality of life.
However, it's important to understand that sinus surgery is not always a permanent "cure." Up to 20% of patients may experience symptom recurrence over time, particularly those with severe chronic sinusitis, extensive polyps, or underlying conditions like allergies or asthma. If symptoms do return, further medical management or, in some cases, revision surgery, may be necessary. For many, even if symptoms recur, they are often less severe and more manageable than before surgery.
The key to long-term success often involves continued medical management, including regular use of saline rinses, prescribed nasal sprays, and ongoing allergy treatment. Think of surgery as creating a clean slate, making other treatments more effective.
Taking the Next Step: Your Path to Clearer Breathing
Understanding sinus surgery and its indications can transform a daunting prospect into a clear path forward. If chronic sinus problems are diminishing your quality of life and conservative treatments have fallen short, a conversation with an otolaryngologist (ENT) is your next, best step. They can accurately diagnose your condition, provide personalized guidance, and help you determine if surgery is the appropriate option for you.
Remember, the goal isn't just to alleviate symptoms, but to restore proper sinus function, allowing you to breathe easier, sleep better, and reclaim a life free from the constant burden of sinus disease. With proper evaluation, meticulous preparation, skilled surgical care, and diligent post-operative follow-up, a future with clearer breathing and enhanced well-being is within reach.